By ChiroTrust.org on February 13, 2014
The brain is supplied by blood from two arterial sources: the paired internal carotid arteries and the paired vertebral arteries. The blood supply to brain from the carotid arteries is referred to as the anterior circulation to the brain. The blood supply to brain from the vertebral arteries is referred to as the posterior circulation to the brain.
The vertebral arteries are exceptionally unique: they ascend to the brain through an opening, a foramen, in the transverse process of the cervical vertebrae.
This opening is called the foramen transversarium. The foramen transversarium exists in the cervical vertebrae C6-C1. The vertebral arteries ascend in the foramen transversarium before entering the skull through the foramen magnum.
After entering the skull, the paired vertebral arteries merge to become the singular basilar artery (drawing from reference 1).
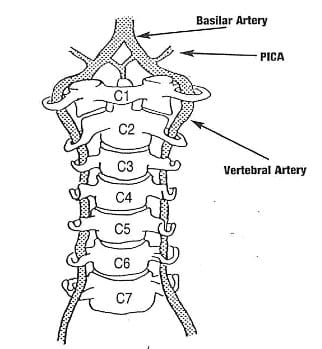
Image from Chiro-Trust.org
The singular basilar artery ascends along the anterior surface of the brain stem, supplying its vascular needs through the pontine arteries. The basilar artery ends when it bifurcates into the paired posterior cerebral arteries (drawing from reference 1).
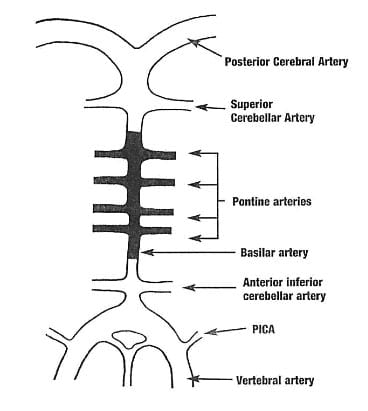
Image from Chiro-Trust.org
The posterior cerebral arteries form the posterior aspect of the Circle of Willis. The Circle of Willis is the unique anatomical location where the posterior circulation (originates with the vertebral arteries) and the anterior circulation (originates with the internal carotid arteries) to the brain amalgamate together.
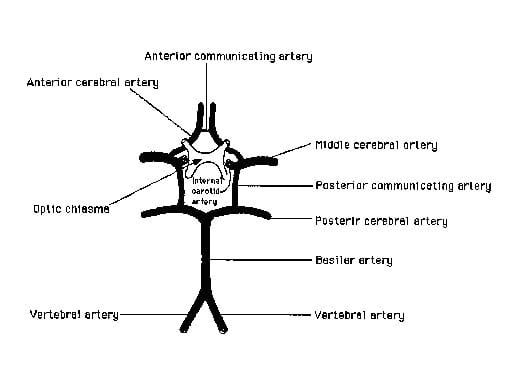
Image from Chiro-Trust.org
The atlas-axis (C1-C2) vertebral articulation of the cervical spine is mechanically unique. It is designed for the function of rotational motion. When one maximally turns one’s head, approximately 55% of that motion occurs at the atlas-axis articulation. The vertebral artery in the foramen transversarium between the atlas and axis must accommodate this rotational motion. This places the vertebral artery at increased risk of tractional types of stress and potential injury as a consequence of a variety of upper cervical spine mechanical loads.
The potential tractional injury to the vertebral artery is a dissection, and usually referred to as vertebral artery dissection, or VAD.
Right cervical spine (head) rotation, showing the tension on the left vertebral artery between the atlas and axis (drawing from reference from 1).
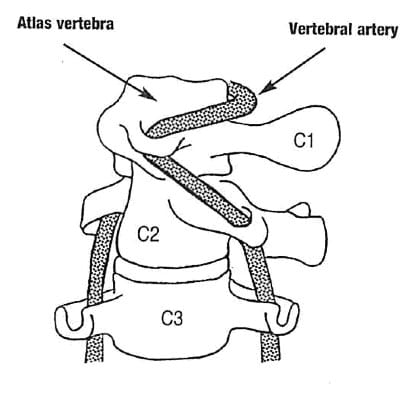
Image from Chiro-Trust.org
Cervical arterial dissection is one of the main causes of ischemic stroke in young adults. Cervical arterial dissections can be categorized as traumatic or spontaneous. Cervical artery dissections occur when a tear forms in the tunica intima and blood enters into the space between intima and media. This can lead to a complete occlusion of the vessel lumen, which is mostly followed by recanalization after several months (2).
Approximately 2/3 of cervical artery dissections are spontaneous and approximately 1/3 of them are posttraumatic. The overall annual incidence of spontaneous and posttraumatic dissections of the carotid artery is 26 / 1 million. The incidence of vertebral arterial dissection (spontaneous and posttraumatic) is 15 / 1 million. As noted, spontaneous cervical artery dissections occur twice as often as posttraumatic cervical artery dissections (2).
Signs and symptoms that would warn of a possible vertebral artery dissection with ischemia are often summarized as the 5 Ds And the 3 Ns (1):
Dizziness (vertigo, light-headedness)
Drop attacks
Diplopia (or other visual problems)
Dysarthria [Speech Disorder]
Dysphagia [Difficult or Painful Swallowing]
Ataxia of gait (Hemiparesis)
Nausea (possibly with vomiting)
Nystagmus
Numbness (hemianesthesia)
A history that would warn of a possible vertebral artery dissection with ischemia involves a sudden onset of severe head and/or neck pain, which is like no other pain the patient has previously suffered. This is especially important if the patient can isolate the pain to the suboccipital region (1).
According to a review of the literature by Alan Terrett (1), a number of non-manipulative mechanical events have been linked to vertebral artery dissections. These mechanical events usually involve rotation and/or extension, and include:
Childbirth
By Surgeon or Anesthetist During Surgery
Calisthenics, Athletics, Fitness Exercise
Yoga
Overhead Work, Painting a Wall
Hanging Out the Washing
Neck Extension during Radiography
Neck Extension for a Bleeding Nose
Turning the Head while Driving a Vehicle
Tonic Clonic Convulsive Seizure
Amusement Park Ride
Protracted Dental Work
Archery
Sneezing/Nose Blowing/Coughing
Wrestling
Emergency Resuscitation
Star Gazing, Watching Aircraft
Sleeping Position
Swimming
Break Dancing
Football
Beauty Parlor Stroke, Sitting in a Barber’s Chair
Tai Chi
Sexual Intercourse
With respects to risk of vertebral artery dissection associated with cervical manipulation, all chiropractors are well aware of the issue. Vertebral artery dissection is extensively discussed in both chiropractic undergraduate and post graduate continuing educational programs. Entire books are written on the subject and are a part of core curriculum at chiropractic colleges (1). Chiropractors are well schooled on the pertinent anatomy, signs/symptoms, clinical presentations, examination findings, and procedures that may possibly be associated with increased risk. Although the risk of vertebral artery dissection is quite rare (as infrequent as 1/ 3,800,000 cervical manipulations in one study (4)), it appears to have a higher risk with the coupling of rotation with extension of the atlas (C1) on the axis (C2).
In an important article published in 1995 (3), Alan Terrett reviewed the published literature pertaining to the incidence of reported adverse events associated with chiropractic spinal adjusting (manipulation). Astonishingly, his results revealed that in many of the published adverse events ascribed to chiropractic manipulation were, in fact, not associated with chiropractic in any manner. Apparently, the authors of the articles assumed “chiropractic” and “manipulation” were synonyms. When untrained laypersons or physicians performed a manipulation resulting in a reported adverse event, authors would claim that the manipulation was performed by a chiropractor. The list of discovered manipulators included:
A Blind Masseur
An Indian Barber
A Wife
A Kung-Fu Practitioner
Self Manipulation
Often the manipulation was performed by a medical doctor, an osteopath, a naturopath, or a physical therapist.
Dr. Terrett concluded:
“This study reveals that the words chiropractic and chiropractor commonly appear in the literature to describe spinal manipulative therapy, or practitioner of spinal manipulative therapy, in association with iatrogenic complications, regardless of the presence or absence of professional training of the practitioner involved.”
“The words chiropractic and chiropractor have been incorrectly used in numerous publications dealing with spinal manipulative therapy injury by medical authors, respected medical journals and medical organizations.”
“In many cases, this is not accidental; the authors had access to original reports that identified the practitioner involved as a non-chiropractor. The true incidence of such reporting cannot be determined.”
“Such reporting adversely affects the reader’s opinion of chiropractic and chiropractors.”
“It has been clearly demonstrated that the literature of medical organizations, medical authors and respected, peer-reviewed, indexed journals have, on numerous occasions, misrepresented the facts regarding the identity of a practitioner of manual therapy associated with patient injury.”
“Such biased reporting must influence the perception of chiropractic held by the reader, especially when cases of death, tetraplegia and neurological deficit are incorrectly reported as having been caused by chiropractic.”
“Because of the unwarranted negative opinion generated in medical readers and the lay public alike, erroneous reporting is likely to result in hesitancy to refer to and underutilization of a mode of health care delivery.”
In 2002, Dr. Scott Haldeman from the Department of Neurology, University of California, Irvine, and colleagues, published a study titled (5):
“Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation”
The study, published in Spine, was a retrospective review of 64 medicolegal records describing cerebrovascular ischemia after cervical spine manipulation. The authors note, that up to 2002, only about “117 cases of post-manipulation cerebrovascular ischemia have been reported in the English language literature.”
The authors further indicate that proposed risk factors for cerebrovascular ischemia secondary to spinal manipulation include age, gender, migraine headaches, hypertension, diabetes, birth control pills, cervical spondylosis, and smoking, and that it is often assumed that these complications may be avoided by clinically screening patients and by pre-manipulation positioning of the head and neck to evaluate the patency of the vertebral arteries. However, after an extensive review, these authors conclude:
“This study was unable to identify factors from the clinical history and physical examination of the patient that would assist a physician attempting to isolate the patient at risk of cerebral ischemia after cervical manipulation.”
“Cerebrovascular accidents after manipulation appear to be unpredictable and should be considered an inherent, idiosyncratic, and rare complication of this treatment approach.”
In 2008, Dr. David Cassidy and colleagues published the most comprehensive study to date pertaining to the risk of vertebral artery dissection as related to chiropractic cervical spine manipulation (6). The article was published in Spine, and titled:
“Risk of Vertebrobasilar Stroke and Chiropractic Care:
Results of a Population-Based Case-Control and Case-Crossover Study”
Key points from this article include:
1) “Vertebrobasilar artery stroke is a rare event in the population.”
2) “We found no evidence of excess risk of vertebral artery stroke associated chiropractic care.”
3) “Neck pain and headache are common symptoms of vertebral artery dissection, which commonly precedes vertebral artery stroke.”
4) “The increased risks of vertebral artery stroke associated with chiropractic and primary care physicians visits is likely due to patients with headache and neck pain from vertebral artery dissection seeking care before their stroke.”
5) Most cases of vertebral arterial dissection occur spontaneously.
6) “Because patients with vertebrobasilar artery dissection commonly present with headache and neck pain, it is possible that patients seek chiropractic care for these symptoms and that the subsequent vertebral artery stroke occurs spontaneously, implying that the association between chiropractic care and vertebral artery stroke is not causal.”
7) “Since it is unlikely that primary care physicians cause stroke while caring for these patients, we can assume that the observed association between recent primary care physician care and vertebral artery stroke represents the background risk associated with patients seeking care for dissection-related symptoms leading to vertebral artery stroke. Because the association between chiropractic visits and vertebral artery stroke is not greater than the association between primary care physicians visits and vertebral artery stroke, there is no excess risk of vertebral artery stroke from chiropractic care.”
8) Neck manipulation “is unlikely to be a major cause” of these rare vertebral artery stroke events.
9) “Our results suggest that the association between chiropractic care and vertebral artery stroke found in previous studies is likely explained by presenting symptoms attributable to vertebral artery dissection.”
10) “There is no acceptable screening procedure to identify patients with neck pain at risk of vertebral artery stroke.”
In 2004, the American Academy of Orthopedic Surgeons published a monograph titled Neck Pain (7). The second to last chapter in the monograph, chapter 7, is titled:
“Manual Therapy Including Manipulation For Acute and Chronic Neck Pain”
The editor of the monograph is Jeffery Fischgrund, MD, from the Department of Orthopaedic Surgery at William Beaumont Hospital in Royal Oaks, Michigan. This monograph has twelve respected contributors, including the authors of chapter 7, Scott Haldeman, Clinical Professor of Neurology at the University of California, Irvine, and Eric Hurwitz, Associate Professor of Epidemiology at the University of California, Los Angeles. With respect to the safety of spinal manipulation, the authors make the following comments:
“Major complications from manual therapies are extremely rare but, nonetheless, have been a source of much discussion.”
“Estimates of vertebral artery dissections or stroke rates associated with cervical manipulation have ranged form 1 per 400,000 to 1 per 10 million manipulations.”
“An estimate of 1 per 5.85 million manipulations, based on 1988 to 1997 medical record and chiropractic malpractice data from Canada, reflects the experience of practitioners of manipulation.”
“No serious complications from spinal manipulation or other chiropractic forms of manual treatment have been reported from any of the published clinical trials involving manipulation or mobilization for neck pain.”
“It should be noted that complications rates from medications, surgery, and most other neck pain treatments for which data are available are estimated to be higher than those from manual and manipulative therapies.”
Whiplash Trauma and Vertebral Artery Dissection
On January 1, 2011, I performed a PubMed search of the National Library of Medicine database using the words “whiplash AND vertebral artery” and 60 titles were produced. The first published study was dated in 1961.
A 1991 study reported on three cases of posttraumatic vertebral artery dissection (8). All patients were young or middle-aged (range 27 to 49 years). Pain preceded neurological symptoms from hours to six weeks.
In 1995, a study from Jefferson Medical College assessed the occurrence rate for vertebral artery injury after acute cervical spine trauma using MR angiography (9). The authors found that 24% (9/37) of those suffering from acute nonpenetrating cervical spine trauma had sustained vertebral artery injuries. The authors concluded:
“Vertebral artery injuries due to major cervical spine trauma as determined by MR angiography are common. Although these vascular abnormalities usually remain clinically occult, a small percentage of patients may suffer devastating neurologic complications of posterior fossa infarction. Noninvasive assessment of the vertebral arteries by means of MR imaging should be an integral part of the evaluation of the acutely injured cervical spine.”
Also in 1995, a study published in the journal Stroke reports on a case of lethal basilar thrombotic embolus that occurred 2 months after the patient’s injury in a vehicle collision (10). His complaints were headache and episodic visual disturbances. Two months after the accident he suddenly lost consciousness and died. The autopsy revealed a lesion of the right vertebral artery was found at the level of the atlantoaxial joint. The authors concluded:
“We suggest that in patients with disturbances of the vertebrobasilar circulation, attention should be paid to occurrence of [whiplash] neck trauma in the preceding 3 months. Further, anticoagulant therapy should particularly be considered in patients who after suffering neck injuries develop signs of transient ischemic attacks with origin from the posterior cerebral circulation.”
In 1997, researchers from Yamaguchi University School of Medicine in Japan showed that cadaver vertebral arteries sustain significant stretch and elongation during the whiplash trauma (11). The vertebral artery was shown to exceed its physiological range at even low levels of acceleration.
A year later, 1998, researchers from Yale University School of Medicine confirmed that whiplash mechanics persistently and quickly causes excessive elongation of the vertebral artery (12).
In 2000, the European Journal of Emergency Medicine presented a case study of a patient who had headache and neck pain after whiplash injury and subsequently developed cerebellar infarction due to vertebral artery dissection (13). This patient’s pain was out of proportion to his apparent injury and it was a clue to the final diagnosis. The authors opined that gross motor examination for spinal cord injury may not be adequate for patients with minor neck trauma because of the risk of vertebral artery dissection, and therefore detailed cranial nerve and cerebellar examination should be performed for detection of circulatory insufficiency.
In 2002, the journal Neurological Research (14) published an investigational study of the incidence of vertebral artery dissection following minor whiplash trauma. The authors found the incidence to be 24% (7/29).
In 2006, researchers from Yale University School of Medicine exposed cadaver cervical spines to rear-end low acceleration mechanical events (15). They determined that “Elongation-induced vertebral artery injury is more likely to occur in those with rotated head posture at the time of rear impact, as compared to head-forward.”
In 2007, researchers once again from Yale University School of Medicine exposed cadaver cervical spines to frontal and side impact low acceleration mechanical events (16). They determined that “Elongation-induced vertebral artery injury is more likely to occur during side impact as compared with frontal impact.”
Last year (2010), a study published in the journal European Neurologyretrospectively analyzed the data on 500 consecutive patients with whiplash injury and discovered that the incidence of cervical arterial dissections in patients with whiplash injury was much higher than the overall incidence of cervical arterial dissections in the general population (17). They conclude that there is a “causal relationship between arterial dissection and cervical spine distortion injury.”
The authors noted that cervical arterial dissection can become symptomatic months after a whiplash injury. In this study, 37.5% occurred between 4 -12 months post whiplash injury.
These authors make these comments:
“Whiplash trauma in a road traffic accident can lead to cervical arterial dissection, which initially is asymptomatic.”
“Most clinicians are not aware that patients with arterial dissections are still at risk of cerebrovascular events months after the dissection.”
“Dissections of cervical arteries following car accidents are often not recognized by clinical examination.”
“Many dissections of cervical arteries remain clinically asymptomatic, and the association with a car accident is not recognized.”
“The clinical implementation of this finding should be that the patients with whiplash injury acquired in a car accident are screened for arterial dissections. In case of clinically suspected cervical arterial dissection, each patient should receive Doppler sonography.”
“Initial MRI of the cervical spine and follow-up investigations after 1–3 months should be considered in patients with whiplash trauma in order to detect vascular, osseous, ligamentous and nerve injuries.”
In this study, the authors found that head-on collisions and rear-end collisions were equally likely to produce a cervical artery dissection; and that low speed collisions were just as likely as higher speed collisions to create a post-traumatic cervical artery dissection. Most importantly, they found that there is an increased risk of posttraumatic cervical artery dissection within 12 months after whiplash injury by about 400 times compared to the uninjured population. Car accidents are an important risk factor for arterial dissections. The victims of car accidents should be screened for arterial dissections.
Lastly, in 2005, Drs. Michael Haneline and John Triano published a review of the literature comparing the incidence of cervical artery dissection between cervical chiropractic manipulation versus whiplash motor vehicle collision. They conclude:
“Long-lasting abnormalities of blood flow velocity within the vertebral artery have been reported in patients following common whiplash injuries, whereas no significant changes in vertebral artery peak flow velocity were observed following cervical chiropractic manipulative therapy.”
“Perceived causation of reported cases of cervical artery dissection is more frequently attributed to chiropractic manipulative therapy procedures than to motor vehicle collision related injuries, even though the comparative biomechanical evidence makes such causation unlikely.”
“The direct evidence suggests that the healthy vertebral artery is not at risk from properly performed chiropractic manipulative procedures.”
SUMMARY
No therapeutic intervention is without risk. The risk of vertebral artery dissection as a consequence of upper cervical spine manipulation is extremely rare. When untrained individuals attempt spinal manipulation, there is an increased incidence of adverse events. For decades, chiropractors have been taught about the potential for vertebral artery injury with certain manipulative maneuvers, and are extremely well trained in the effective delivery of safe spinal manipulations. Newer evidence has even questioned if there is any increased risk of cervical artery dissection as a consequence of chiropractic cervical spine manipulation, yet they remind the practitioner that the symptoms associated with spontaneous vertebral artery dissection may bring the patient into their offices (6).
In contrast, there is significant evidence that a much greater risk for vertebral artery dissection (400 times higher) exists as a consequence of whiplash motor vehicle collisions (17). The evidence clearly shows that during whiplash mechanics, the vertebral artery sustains significant abnormal stretch and injurious elongation. Post-whiplash vertebral artery injury can be asymptomatic for months following the collision, yet it can result in catastrophic outcomes, including death. The evidence supports that all whiplash-injured patients should be observed for symptoms and/or signs of vertebral-basilar insufficiency for months following injury; if any such symptoms and/or signs present, additional diagnostics are warranted, and the statistical etiology should be understood.
REFERENCES
1) Terrett AGJ; Current Concepts in Vertebrovascular Complications Following Spinal Manipulation; Second Edition; NCMIC Group, 2001.
2) Hauser V, Zangger P, Winter Y, Oertel W, Kesselrin J; Late Sequelae of Whiplash Injury with Dissection of Cervical Arteries; European Neurology; August 18, 2010, Vol. 64, No. 4, pp. 214–218.
3) Terrett AG; Misuse of the literature by medical authors in discussing spinal manipulative therapy injury; Journal of Manipulative and Physiological Therapeutics; 1995 May;18(4):203-10.
4) Carey PF; A report on the occurrence of cerebrovascular accidents in chiropractic practice; Journal of the Canadian Chiropractic Association; June 1993, Vol. 37, No. 2, pp. 104-106.
5) Haldeman S, Kohlbeck FJ, McGregor M; Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation; Spine; 2002 Jan 1;27(1):49-55.
6) Cassidy, J David DC, PhD; Boyle, Eleanor PhD; Côté, Pierre DC, PhD; He, Yaohua MD, PhD; Hogg-Johnson, Sheilah PhD; Silver, Frank L. MD; Bondy, Susan J. PhD; Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-Based Case-Control and Case-Crossover Study; Spine; Volume 33(4S), February 15, 2008 pp S176-S183.
7) Fischgrund, JS; Neck Pain, American Academy of Orthopedic Surgeons, 2004.
8) Hinse P, Thie A, Lachenmayer L. Dissection of the extracranial vertebral artery: report of four cases and review of the literature. Journal of Neurology, Neurosurgery and Psychiatry. 1991 Oct;54(10):863-9.
9) Friedman D, Flanders A, Thomas C, Millar W. Vertebral artery injury after acute cervical spine trauma: rate of occurrence as detected by MR angiography and assessment of clinical consequences. American Journal of Roentgenology. 1995 Feb;164(2):443-7.
10) Viktrup L, Knudsen GM, Hansen SH. Delayed onset of fatal basilar thrombotic embolus after whiplash injury. Stroke. 1995 Nov;26(11):2194-6.
11) Nibu K, Cholewicki J, Panjabi MM, Babat LB, Grauer JN,Kothe R, Dvorak J. Dynamic elongation of the vertebral artery during an in vitro whiplash simulation. European Spine Journal. 1997;6(4):286-9.
12) Panjabi MM, Cholewicki J, Nibu K, Grauer JN, Babat LB,Dvorak J. Mechanism of whiplash injury. Clinical Biomechanics (Bristol, Avon). 1998 Jun;13(4-5):239-249.
13) Chong CL, Ooi SB. Neck pain after minor neck trauma–is it always neck sprain? European Journal of Emergency Medicine. 2000 Jun;7(2):147-9.
14) Chung YS, Han DH. Vertebrobasilar dissection: a possible role of whiplash injury in its pathogenesis. Neurological Research. 2002 Mar;24(2):129-38.
15) Ivancic PC, Ito S, Tominaga Y, Carlson EJ, Rubin W, Panjabi MM. Effect of rotated head posture on dynamic vertebral artery elongation during simulated rear impact. Clinical Biomechanics (Bristol, Avon). 2006 Mar;21(3):213-20.
16) Carlson EJ, Tominaga Y, Ivancic PC, Panjabi MM. Dynamic vertebral artery elongation during frontal and side impacts. Spine Journal. 2007 Mar-Apr;7(2):222-8.
17) Vital Hauser, Peter Zangger, Yaroslav Winter, Wolfgang Oertel, Jung Kesselrin; Late Sequelae of Whiplash Injury with Dissection of Cervical Arteries; European Neurology; August 18, 2010, Vol. 64, No. 4, pp. 214–218.
18) Haneline M, Triano J. Cervical artery dissection. A comparison of highly dynamic mechanisms: manipulation versus motor vehicle collision. Journal of Manipulative Physiological Therapeutics. 2005 Jan;28(1):57-63.