What Causes Acid Reflux?
According to Jonathon V. Wright, MD nearly 100% of patients with heartburn and gastrointestinal complaints do not create enough stomach acid. (1) This may seem odd to hear because we’ve been told for years that too much acid is the culprit for most GI issues like GERD, acid reflux and Americans have been prescribed antacids by the droves because of this theory.
Unfortunately, these drugs do not help cure the organic cause of acid reflux or other GI issues and – although Nexium, Pepcid, Prevacid, Prilosec, Zantac and others to help keep symptoms to a minimum temporarily – they actually do more harm in the long-run!
Dr. Wright, author of “Why Stomach Acid is Good for You,” explains the reason why. Contrary to popular belief, he discovered that literally half of the American populationover 50 years old lacks the appropriate amount of stomach acid to digest their food fully has to do with us not understanding how our stomach and digestive tract actually work. (2)
In this article, you will learn what causes acid reflux and the diet and remedies to treat it!
How the Stomach Works
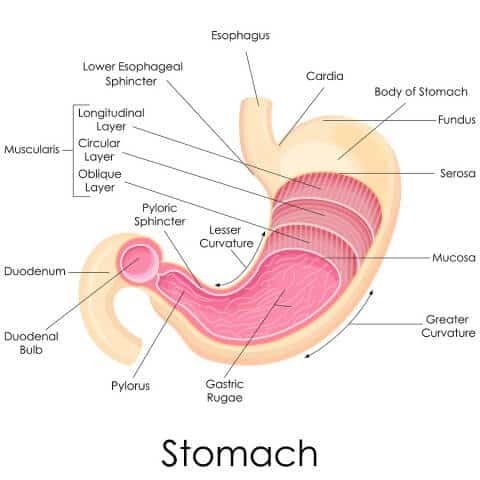
The stomach is a fascinating organ that is lined with mucus-secreting cells and two important glands: gastric glands, which secrete hydrochloric acid, intrinsic factor, mucus and pepsinogen; and pyloric glands, which mainly secretes mucus that protects the stomach from hydrochloric acid.
Under continuous control by hormones and nervous system signals, there are three phases to this process:
- Cephalic Phase – When you think about, smell, or taste food about 20% of the gastric secretions are created before food even enters your stomach.
- Gastric Phase – Every time you eat, the food in your stomach triggers parietal cells to release the highly acidic hydrochloric acid (0.8 pH).
- Intestinal Phase – When food enters your small intestines, the duodenum produces small amounts of gastric juices.
Ultimately, it’s the acid that breaks down proteins into key nutrients and amino acids, which explains why people with low stomach acid can struggle with insufficient neurotransmitter-related diseases like anxiety, depression and even Parkinson’s disease. In one study, it was even discovered that up to 60% of Parkinson’s patients had proven decreased gastric acid secretion! (3)
What Causes Acid Reflux
As I mentioned above, too much stomach acid is NOT the cause of acid reflux. The primary cause of heart burn and GERD is that acid enters the esophagus because of a leaky valve. There are a variety of reasons it happens, but essentially the esophageal valve that connect the esophagus and stomach is unable to shut properly and gastric juices end up “sneaking up the pipe” so to speak. Some common causes include:
-
Hiatal hernia – Normally, the diaphragm helps keep acid from rising into the
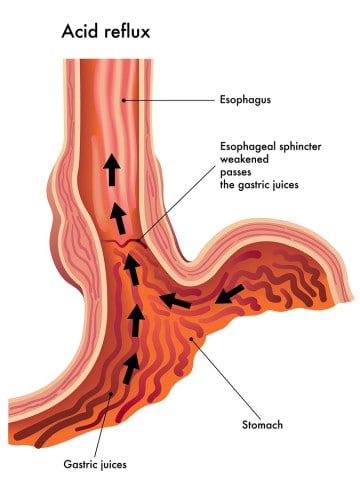 esophagus. However, if the upper part of the gut moves above this muscle that separating the chest from the stomach, acid can leak through.
esophagus. However, if the upper part of the gut moves above this muscle that separating the chest from the stomach, acid can leak through. - Pregnancy – The excess pressure from the growing fetus can sometimes be too much for the esophageal valve.
- Smoking – Shown to damage mucus membranes, impair muscle reflexes, increase acid secretion, and reduce salivation smoking can lead to acid reflux.
- Too little acid – Completely contrary to what is commonly taught today, too little stomach acid causes a slew of GI issues like leaky gut that contribute to acid reflux.
- Eating before bed -Eating too close to bedtime and then laying down puts your body in a position that is abnormal for digestion which can cause acid reflux.
- Excessive exercise – Doing lots of long distance cardiovascular exercise like marathons can make it harder to digest the food you eat.
- Taking medications – Drugs like aspirin, ibroprofen, muscle relaxers, blood pressure medications, steroids and anti-biotic drugs can damage the gut lining causing acid reflux.
- Being overweight or obese – Putting on extra body weight can cause acid reflux by increasing pressure on your esophageal valve and may also be linked to low stomach acid.
In addition, here are common acid reflux food triggers:
- Alcohol
- Carbonated beverages
- Chocolate
- Citrus fruits
- Coffee
- Desserts
- Fried foods
- Spicy foods
- Tomato products
If you have acid reflux, look to restrict these foods as part of your acid reflux diet.
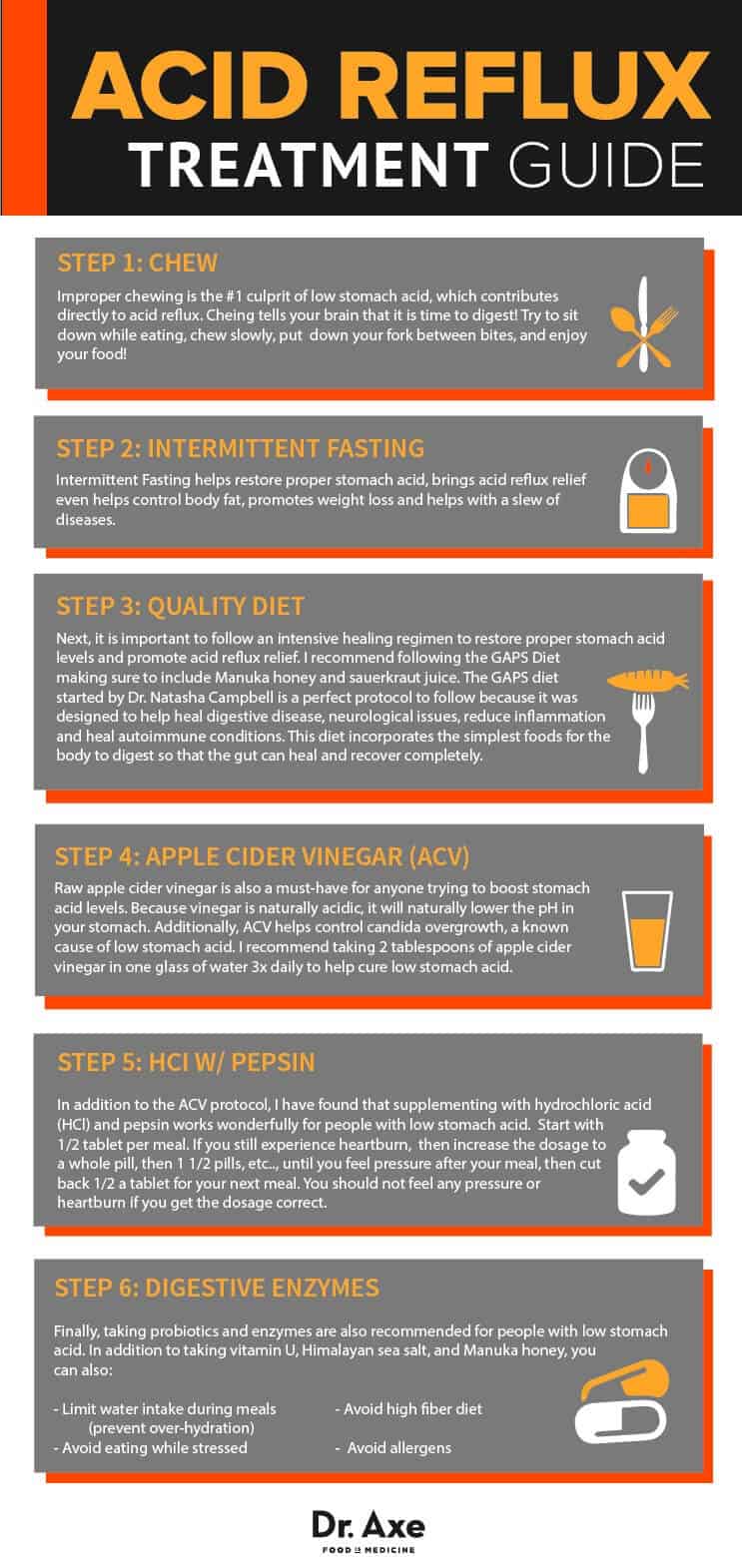
Step-by-Step Guide to Heal Acid Reflux
Healing low stomach acid-related conditions isn’t that difficult, but it does take some determination and resolve. I have found that when my patients follow this step-by-guide their issues quickly melt away.
![]()
1. Chew
First and foremost, in my opinion improper chewing is the #1 culprit explaining why people have low stomach acid. While chewing food, neurogenic signals originating in the cerebral cortex and appetite centers of the amygdala and hypothalamus transmit messages through the dorsal motor nuclei of the vagus nerve to the stomach. (4)
When people scarf down their food and only take a few bites, this processes is considerably shortened and the gastric secretions associated with the cephalic phase described above will be greatly diminished.
There’s no hard or fast rule to follow, but just make sure that you chew thoroughly enough so that the food in your mouth is a soft pasty consistency before you swallow it. This will also help prevent overeating and will promote weight loss!
This past January, for the example, The Journal of the Academy of Nutrition and Dietetics published an article uncovering that eating slowly not only lowers eating rate and energy density in normal and overweight individuals, “Eating slowly led to lower hunger ratings in both groups and increased fullness ratings in the normal-weight group at 60 minutes from when the meal began.” (5)
2. Intermittent Fasting
The benefits of intermittent fasting have been experienced since the beginning of time because, unlike today, food wasn’t readily available around the clock.
Most intermittent fasting techniques center on not eating early in the morning or late at night, and consuming the entire day’s worth of calories during a 4-5 hour window in the middle of the day.
In addition to helping restore proper stomach acid levels and acid reflux relief, researchers have been evaluating the effectiveness of intermittent fasting to control body fat, promote weight loss and help with a slew of diseases for nearly 75 years.
Just last October, for instance, the British Journal of Nutrition published a clinical trial that took 115 overweight women with a family history of breast cancer and restricted their eating via intermittent fasting verses a generic daily calorie been shown to result in greater improvements in insulin sensitivity and weight control than generic daily calorie restriction. (6)
3. Quality Diet
Next, it is important to follow an intensive healing regimen to restore proper stomach acid levels and promote acid reflux relief. I recommend following the GAPS Diet making sure to include Manuka honey and sauerkraut juice.
The GAPS diet started by Dr. Natasha Campbell is a perfect protocol to follow because it was designed to help heal digestive disease, neurological issues, reduce inflammation and heal autoimmune conditions. This diet incorporates the simplest foods for the body to digest so that the gut can heal and recover completely.
4. Apple Cider Vinegar (ACV)
Raw apple cider vinegar is also a must-have for anyone trying to boost stomach acid levels. Because vinegar is naturally acidic, it will naturally lower the pH in your stomach.
Additionally, ACV helps control candida overgrowth, a known cause of low stomach acid. I recommend taking 2 tablespoons of apple cider vinegar in one glass of water 3x daily to help cure low stomach acid.
5. HCl w/ Pepsin
In addition to the ACV protocol, I have found that supplementing with hydrochloric acid (HCl) and pepsin works wonderfully for people with low stomach acid.
Start with 1/2 tablet per meal. If you still experience heartburn, then increase the dosage to a whole pill, then 1 1/2 pills, etc. until you feel pressure after your meal, then cut back half a tablet for your next meal. You should not feel any pressure or heartburn once you get the dosage correct.
As a word of caution: Do NOT use HCL supplements if you take corticosteroids or anti-inflammatory medications such as NSAIDS (Advil or Tylenol). These drugs oftentimes damage the GI lining and put your at risk of developing stomach ulcers, which will be exacerbated if you take HCL.
IMPORTANT: It is very important to eat at least a small amount of protein with each meal. HCl primarily helps break down your proteins, so you want to give your stomach something to breakdown. Eggs, lean proteins, or soaked nuts and seeds (once you get past the introductory diet on GAPS).
6. Digestive Enzymes
Finally, taking probiotics and enzymes are also recommended for people with low stomach acid. They are both extremely useful in digesting food, which takes the burden off of your GI system while it heals.
Because American diets are low in probiotics, most people find it helpful to keep supplementing with probiotic/enzyme long after their low stomach acid heals.
In addition to taking vitamin U, Himalayan sea salt, and Manuka honey, here are some other tips to restore proper stomach acid levels:
- Limit water intake (preventing over-hydration)
- Avoid high fiber diet
- Avoid allergens
- Not eating while stressed
Acid Reflux Medication Side Effects
It is important to remember that this entire process of digestion is controlled by multiple body systems, and what happens in your gut determines the function of your entire body! This explains why people taking drugs to stop or reverse stomach acid production oftentimes experience a wide range of symptoms seemingly unrelated to stomach acid.
The perfect example can be seen when proton pump inhibitors (PPI) are prescribed. Reducing the production of acid by blocking key enzymes in the stomach lining that produce acid, conventional medicine teaches that PPI’s helps prevent ulcers or gastroesophageal reflux disease (GERD), and that the reduction in stomach acid creates an internal GI environment where the body can heal itself of these conditions.
Sadly, this is simply not the case.
Being virtually useless because most GI issues are connected to low stomach acid, Prevacid and other proton pump inhibitors PPI’s have been linked to a wide range of side effects, which adds insult to injury and contribute even more to what causes acid reflux. Some of the common side effects are: (3)
- Confusion and dizziness
- Constipation and diarrhea
- Coughing and a choking sensation
- Feelings of being “jittery”
- Headache
- Nausea and stomach pain
- Muscle cramps and muscle weakness
- Rapid heart rate
- Seizures
- Spastic muscle movements
Additionally, people taking PPIs to lower stomach acid will oftentimes experience other health concerns:
- Improper protein metabolism
- Imbalanced gut flora
- Nutrient malabsorption
- Leaky gut & food allergies
When healing what causes acid reflux and low stomach acid, be diligent to follow these few simple steps and you’re certain to see fantastic results in no time flat!